Wearable sensors can facilitate a shift from reactive treatment of a disease to proactive prevention. In an age of chronic disease management, they can help to monitor patients’ realworld behavior. But sponsors face challenges implementing wearable sensors in clinical trials. Before sponsors can implement digital endpoints in their studies, they must first validate the endpoints (and their algorithms). To gain greater insights into patients’ health, sponsors should leverage wearable sensor platforms designed for clinical trials, collect raw data, and utilize open-source algorithms.

Wearable sensors have the potential to transform healthcare. In many instances, wearable sensors can pick up signs that a person is getting sick before even they realize it. This capability is particularly relevant for chronic conditions. Imagine sensors picking up signs of worsening heart disease in Congestive Heart Failure (CHF) patients and spurring an intervention before the patient needs to be readmitted to the hospital. Wearable detected changes in a person’s gait can already predict an increased risk of falls – a major cause of hospitalization and death in the elderly – and enable proactive interventions to be made.
The potential healthcare cost reductions and quality-of-life benefits this could produce are enormous. With aging populations around the world, chronic disease management increasingly dominates healthcare spending. In fact, 86% of healthcare spending in the U.S. was on adults with chronic conditions, according to a study published in ACR Open Rheumatology in February 2020. While COVID had a major temporary impact on the proportion of resources devoted to infectious disease, there is little question that chronic conditions are the biggest long-term healthcare concern.
The ability to forecast health issues can transform healthcare from reactive treatment to proactive prevention of illness – arguably the most fundamental change in the history of healthcare. Furthermore, these capabilities can be used to assess treatments in real-world situations, potentially transforming clinical trials.
The increasing dominance of chronic diseases affects clinical trials. According to 2016 research from the Tufts Center for the Study of Drug Development, it cost $2.6 billion to bring a drug to market: a 145% increase over 10 years. While some question Tufts’ methodology, there is no question about the trend. One major driver of this increase is the increased incidence of chronic diseases.
Unlike other diseases where outcomes (e.g., cure and mortality rates) can be objectively measured, chronic diseases tend to be characterized by the degree of severity. Many studies still rely on subjective measures – like doctors asking patients how they feel or how much pain they experience – to gauge the quality of life. Not only are these measures highly subjective; but they are also prone to recency bias, where patients place too much weight on experiences in the past 1-2 days. These measures are unreliable and uncertain.

To get more reliable data, clinical trials have resorted to larger sample sizes, driving up costs and prolonging trials. Often, that is still not enough. Most pharmaceutical companies have placed their hope in drugs that looked promising in Phase 2 trials, only to witness them fail in Phase 3.
The pressure to contain costs also stems from diminishing returns in a crowded market. Just about every condition already has an existing treatment – many of which are quite good. As a result, the incremental increased value from new treatments is getting smaller. Profits are getting squeezed. Return on pharma R&D was at 1.9%, according to one 2018 Deloitte study. That’s less than a U.S. Treasury bond. No company will continue to invest for long at those rates of return.
Wearables can measure digital endpoints that address these challenges. They can redefine the success of clinical trials and transform them. Occasional, often subjective, measures of patient progress – such as patient-reported outcomes or in-clinic tests – can be replaced. Instead, wearable sensors can provide continuous documentation of a patient’s progress. For example, an activity monitor worn by a patient with Parkinson’s disease or chronic obstructive pulmonary disease (COPD) can determine quantitatively whether their activity level is increasing or decreasing over time. It can even provide detailed gait metrics and analysis of freezing periods. This data can be measured and monitored 24 hours a day, 7 days a week. Objective measurement replaces subjective. A continuous perspective supersedes episodic glimpses.
These changes can improve the reliability of clinical trial data and reduce measurement uncertainty. They bring about manifold benefits. For example, they reduce the likelihood of incorrect assessments from clinical trials. Accordingly, this reduces the required sample size, potentially shortening the duration of the trial, and helping to contain the rising cost of drug development. Similarly, continuous monitoring makes it possible to detect an unexpected deterioration in overall health. Adverse events can potentially be identified earlier. For healthcare providers, this improved feedback can inform a potential course correction. More importantly, it improves patient safety. Furthermore, data from wearables can be monitored remotely, potentially reducing the number of visits required to clinical sites and the burden on clinical trial participants. This in turn may contribute to improvements in patient enrollment and retention and mitigate the risk of disruptions to clinical trials.
Employing wearables in clinical trials is not without challenges, which fall into two categories: (A) implementation and (B) interpretation.
Implementing wearables in a clinical trial comes with its own challenges: predominantly training, compliance, and troubleshooting. Trials often involve dozens or hundreds of clinical sites, which manage the deployment of wearable sensors to participants. Often, these sites only enroll a few participants a year. Keeping site staff trained and up to speed on the technology can be a significant challenge, especially if staff turnover is high. Likewise, participants’ compliance with the protocol needs to be managed. Although there are systems that track compliance, monitoring them requires time and training. Finally, technical issues must be identified, diagnosed, and rectified. Building the processes to train, manage compliance, and troubleshoot places additional burdens on sites.
The real challenge lies in using wearable-generated data. There are, currently, very few accepted digital clinical endpoints. Without an accepted endpoint, wearable data cannot be used to advance the goals of a clinical trial. As a result, the adoption of digital technologies in clinical trials is very low. A recent review of the Digital Medicine Society (DiMe) Library of Digital Endpoints identified 325 endpoints used in 155 trials out of the tens of thousands of trials conducted during the same period.
Further review of the DiMe data showed that almost two-thirds (198) of endpoints analyzed three basic concepts: glucose levels (73), activity levels (70), and sleep/nocturnal activity (55). That these indicators were widely used is not the problem; they are important measures of health, and almost any malady likely affects activity and sleep levels. The issue, however, lies with the proliferation of measures that are, essentially, of the same parameters. Many of these measures are based on proprietary (processed) metrics that must be validated independently for every disease for which they are used. And, if the algorithms are modified, validation must be repeated. See sidebar 1 for a discussion of why validating wearable algorithms/endpoints are so challenging. Should regulators and doctors be expected to understand tens or even hundreds of different measures for essentially the same value?
Validation of diagnostic medical devices generally involves proving equivalence to an approved predicate device. For most devices, this means showing that the device provides an equivalent single measurement across all relevant populations (age, sex, race, etc.) and parameters (e.g., heart rate or oxygen level) for which it might be used. This can be a challenge, but it is manageable. Proving substantial equivalence of an algorithm to analyze wearable sensor data is infinitely more difficult. Not only do you need to address the relevant population/ parameter ranges, but you must be able to do it in every context in which it might be used. For example, an activity monitor must provide the same results over every time interval (hour, day, month, etc.) and every type of activity (e.g., sleeping, walking, climbing stairs, climbing a mountain, and playing tennis) to be considered equivalent to another. As a result, validating a wearable algorithm is very difficult.
Fortunately, there are ways to address these challenges. First, sponsors can work with companies whose technology platforms are specifically designed for clinical trials and who provide a full range of support services to help alleviate the implementation challenges. Using purposebuilt technology and expert support minimizes the implementation challenges.
More importantly, sponsors can capture raw sensor data, which establishes a common denominator for addressing the validation challenge. There is some debate over what constitutes raw data, because all sensor output is, strictly speaking, processed by at least an analog to digital converter. We define raw data as (a) minimally processed and (b) able to be verified by independent physical measurement. For example, acceleration measurements constitute raw data; steps are processed data. So long as sensor output can be independently measured, it does not matter that there is some pre-processing. In this context, validating that two wearable sensors provide equivalent raw data is relatively simple. Accelerometers can be placed on a shaker table; optical sensors can be assessed with respect to other validated sensors. In fact, sensor manufacturers typically do this work and provide specific accuracy specifications as part of their product specifications.
Using raw data, it is possible to develop clinical endpoints that are device independent and can be shared across multiple studies. Furthermore, a library of raw data can be used to validate new versions of algorithms without collecting new data. If open-source algorithms are used, validation work from different studies and applications can be combined to extend and support new endpoints.
Capturing the potential of wearable sensors in clinical trials and healthcare in general can seem like a daunting task. We can make it less daunting if we, as an industry, collaborate in precompetitive areas. Two areas are particularly ripe for precompetitive collaboration. The first is to standardize digital endpoints. Regulators and healthcare providers cannot be expected to understand and accommodate many different ways to measure essentially the same phenomena, like activity level or sleep quality. By standardizing these measures, we can leverage the work of others and reduce confusion in the field. We believe that using open-source algorithms is the best approach, given the challenges of proving substantial equivalence of continuous digital endpoints, but any step towards standardization would be useful.

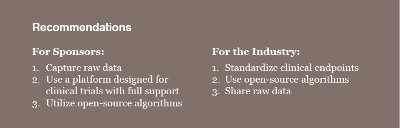
Perhaps even more important is to find a way to systematically share raw sensor data that are connected to reliable independent health outcomes. Collecting the data is by far the most expensive part of discovering and validating digital endpoints. Much data is already being collected, but it tends to be highly siloed and never shared. As a result, new data is collected to discover and validate every digital endpoint – even though researchers are using equivalent sensors. Once collected and used for the particular study, the data are rarely reused – a tremendous waste. Although there are clearly privacy, security, and competitive concerns with data sharing, these can be overcome. The value of precompetitive data sharing is too high for us to continue to work without it.
References